![]()
.
Ebola Or African Strains Of TB? © U.S. Library of Congress |
|
“Diagnosing Ebola in a person who has been infected for only a few days is difficult, because the early symptoms, such as fever, are nonspecific to Ebola infection and are seen often in patients with more commonly occurring diseases, such as malaria and typhoid fever.”1 Only a sin of omission. then, would explain why anyone or any group would not want to specifically mention the most commonly occurring cause of infectious death in Africa — tuberculosis — whose sky-high rates in West Africa make Ebola look like a dropper-full of water squeezed into the Mississippi. If by October, 2014, Ebola had laid claim to what WHO (the World Health Organization) claimed was well over 4,000 deaths since its February outbreak2 — certainly this ought to be weighed in the light of the approximately 600,000 Africans slain by TB during the same window of time.3 Furthermore, if by October 17th, 2014 world-wide Ebola mortality stood at 4,811 then surely 81% of these deaths took place in Liberia and Sierra Leone. While Librarian health officials warned4 as early as 2009 that TB was skyrocketing out-of-control — a mixed scientific coalition from Sierra Leone and Germany cautioned that Sierra Leone’s tuberculosis level was not only the highest in West Africa, but filled with resistant strains of TB and tuberculous Mycobacterium Africanum that had “reached an alarming level”…..raising the question of possible consequences” for a future new TB epidemic.”5 Indeed almost half of all TB cases in the West African Ebola zone are caused by such Mycobacterium africanum — an unusual, yet just as deadly member of the tubercular family, exclusive to West Africa — and fast becoming a microbe of great public — and now global concern. That tubercular M. africanum can and has already caused tuberculosis in the United States is a matter of record.6 Furthermore, there is a body of evidence that M. africanum requires more sustained contact, even among household members—certainly mirrored in the current outbreak. Meanwhile, health officials continue to insist that "casual contact" cannot transmit Ebola—precisely the same claim that they've long made with TB. Surely the CDC is aware that there is not a sign or symptom of Ebola, including its hemorrhagic tendencies that cannot be found in acute disseminated miliary (blood-borne) tuberculosis, once called “galloping consumption” — the single most feared form of the disease ever. And most likely it is also aware that such tuberculosis has its own viral-like forms, some of which can simulate the Ebola. Such viral TB is generally acknowledged to be TB’s preferred form — as a survival strategy to storm any inclement conditions the microbe might find itself in.7 Then why did the CDC not mention TB, by name, in their short-list of possibilities that could cause Ebola-like symptoms? If such oversight stopped there it would be unremarkable, but it seems to have been carried over in the very design of the most recent CDC-approved tests to detect Ebola.
A River named Ebola
In September of 1978, about 40 years ago, a team — including a 27-year-old fresh out of medical school, who was training as a clinical microbiologist at the Institute of Tropical Medicine in Antwerp, Belgium, received a blue thermos from Zaire. It was filled with the two 5ml. clotted blood specimens of an African-based Flemish nun. The Belgium doctor who sent it, Jacques Courteille, practicing in Kinshasa, included a note saying that he was at a complete loss for the nun’s mysterious, yet deadly illness. Also, could the samples be tested for Yellow Fever? This thermos had traveled from Zaire’s capital city of Kinshasa, on a Sabena commercial flight to Belgium — inside its deliverer’s hand luggage. When the samples were received, Peter Piot, the 27-year-old medical graduate and his colleagues, among other things, placed the blood samples under an electron microscope. To be sure Piot’s interest was virology and a virologist he would soon become, best known for his work on theorizing the ‘viruses’ behind Ebola and AIDS. To this effect he contributed heavily to the voluminous literature that HTLV-1 had a role in AIDS, which it did not. Nevertheless Piot would become a pioneer, and part of the group that included veterinarian Max Myron Essex in trying to define what AIDS was at WHO’s 1985 Conference in Banqui, Africa.
Figure . Dr. Peter Piot
Piot on the Ebola: “We saw a gigantic worm like structure — gigantic by viral standards. It’s a very unusual shape for a virus, only one other virus looked like that and that was the Marburg virus.”8
Figure 2. Piot (on the right), at the Institute of Tropical Medicine, Antwerp, in 1976
But the new “virus” needed a name. Piot relates the interesting tale of how Ebola came to be named as Ebola: “On that day our team sat together late into the night we had also had a couple of drinks discussing the question. We definitely didn’t want to name the new pathogen “Yambuku virus”, because that would have stigmatized the place forever. There was a map hanging on the wall and our American team leader suggested looking for the nearest river and giving the virus its name. It was the Ebola River. So by around three or four in the morning we had found a name. But the map was small and inexact. We only learned later that the nearest river was actually a different one. But Ebola is a nice name, isn’t it?”9 Depends upon how you look at it.
Figure 3. The Ebola River, Circa 1976
Piot’s specimens proved negative for Yellow Fever and he mentions that the tests for Lassa fever and typhoid were also negative. What, then, could it be? Piot: “To isolate any virus material” small amounts of the blood samples were injected into VERO cells and into mice. Several of these mice subsequently and abruptly expired — “a sign that a pathogenic virus was probably present in the blood samples that we had used to inoculate them”.10 The fact that the mice died did not mean that it was at the hands of a “pathogenic virus.” Piot’s boss, Stefaan Pattyn, who Piot admitted “could be a bit of a bully”, supposedly specialized in the study of mycobacteria — tuberculosis and leprosy, yet seemed unaware of the hemorrhagic consequences of acute TB, nor had he taken the time to use special stains and cultures to detect its viral-like cell-wall-deficient forms. Instead Pattyn followed his current passion, shared by Piot. Pattyn had recently worked in Zaire for six or seven years and exotic viral illnesses were now “right up his alley”.11 So Pattyn’s team likewise never really considered a strain of acute miliary TB or its viral cell-wall-deficient forms in his rule-outs for an acute hemorrhagic or epidemic fever — among them Mycobacterium tuberculosis and Mycobacterium africanum.
From Past to the Present The Ebola of its day on steroids, “galloping” acute consumptive tuberculosis could kill in days — the mere memory of which, just a few generations ago, brought terror to the faces of those who had witnessed and were describing it. To Dubos12 “galloping consumption” was not an isolated, but a frequent diagnosis in the 19th and early 20th centuries. And despite persistent myths to the contrary, in the early phase of any new TB epidemic from a new and virulent strain, tuberculosis manifests itself as an acute disease and only much later as the chronic pulmonary tuberculosis that we know in today’s western world. An example of this can be found in the high mortality during the 1918 influenza pandemic, when African-Americans were brought to fight in France during World War I — large numbers of them dying from a fast-tracked tubercular “galloping consumption”. Many often underestimate the speed, contagiousness and ferocity of a TB epidemic. Khomenko’s 1993 study13 should have cemented the notion that the explosive contagiousness of just such Ebola and influenza-like viral forms of tuberculosis are exactly the stuff that previous epidemics and pandemics could have been made of. But it didn’t. In the US, the CDC and NIH seemed to
feel differently, ignoring the historic possibility. There was much
the same viral passion, at that time over “Influenza”, when in
1990, a new multi-drug-resistant (MDR) tuberculosis outbreak took
place in a large Miami municipal hospital. Soon thereafter, similar
outbreaks in three New York City hospitals left many sufferers dying
within weeks. By 1992, approximately two years later, drug-resistant
tuberculosis had spread to deadly mini-epidemics in seventeen US
states, and was reported, not by the American, but the international
media, as out of control. Viral forms of swine, avian and human TB
can be transmitted from one species to another. So can exotic strains
of tuberculosis and Mycobacterium africanum, imported into the
United States through countries such as Liberia. By 1993 the World
Health Organization (WHO) had proclaimed tuberculosis a global health
emergency.14 That emergency has never been
lifted. A fact initially carefully minimized
by certain Ebola ‘authorities’ — and clarified by Feldmann in
the New England Journal (October 9th, 2014 issue)
is that in the current Ebola outbreak “less than half” of the
people infected have visible hemorrhaging.22 This was just
enough to prompt some virologists to rethink Ebola’s designation
from Ebola Hemorrhagic Fever, to the “Ebola virus Disease”. So
much for “hemorrhagic fever.” Yet even then, in a 1978
publication of the Bulletin of the World Health Organization
regarding the 1976 Ebola outbreak in Zaire it was admitted that
hemorrhaging, although from “multiple sites” was “principally
[from] the gastrointestinal tract”.23 But patients with
TB spread to the gastrointestinal tract can also have fever,
abdominal pain, and can have gastrointestinal/rectal bleeding that
patients with Ebola can have. Mortality Rates of Both Diseases about the Same
Meanwhile, The World Health
Organization’s (WHO’s) latest “Situation Report” summed-up
that although the rate of Ebola infections were picking up speed at
an alarming rate in West Africa, the fatality rate was 53% overall,
ranging from 64% in Guinea to just 39% in Sierra Leone.26
If this 53% figure was designed to make the situation more bearable,
it hardly achieved its goals. A Flaw in Diagnostic Test Design?
Critics claimed that the two PCR systems to be used for Ebola testing in such “emergency situations” were unapproved. But there is more. While an instruction booklet issued by the Food and Drug Administration28 showed impressive results for detecting and thereby being positive for known “Ebola” samples — it sadly failed in its inadequate selection of those pathogen’s that might be cross-reacting and therefore making for false positive Ebola tests. The instruction booklet, Version 2, that accompanied the new Ebola assay mentions: “9.2.2.2 Bacterial Cross-Reactivity: Bacterial cross-reactivity of the EZ1 assay was evaluated by testing purified nucleic acid of bacteria that potentially could be infecting the majority of the population. No cross-reactivity was observed in the human DNA or any of the bacteria tested (Table 51).”29 [Bold print theirs] Yes. The only problem being that a glance at Table 51 shows practically every bacteria in existence except for the one subset of pathogens “that potentially could be infecting the majority [of West Africa’s] population” and those pathogens are again — Mycobacteria tuberculosis and its related Mycobacterium africanum. Such diversion is no trivial point. As time went by it became obvious that attempts were in the pipeline to link the pathogenesis of Ebola and AIDS, right down to their sexual transmission (a poorly kept secret is that TB can also be sexually transmitted30). So mistakes made during the AIDS probes would have to be avoided with Ebola. For example, in the past, as the first scientist to propose HIV-virus testing, veterinarian Max Myron Essex knew that tuberculosis and its allied mycobacteria gave a false positive for the HIV virus in his tests in almost 70% of cases. Such cross-reactivity between HIV and tuberculosis was so significant, that it forced Essex31 and his protégé, Congo physician Oscar Kashala, to warn that both the HIV screening test, the enzyme-linked immunosorbent assay (ELISA) and western blot results “should be interpreted with caution when screening individuals with M. tuberculosis or other mycobacterial species.”31 This, of course, automatically meant throwing away HIV serum diagnostics for, according to WHO, at least a third of the people in the known world that WHO (The World Health Organization) has proclaimed presently harbor tubercular infection. So why then was Mycobacterium tuberculosis noticeably excluded from the CDC’s Table 51 and not included in those pathogens tested for cross-reacting and therefore possibly giving false positive tests for the Ebola? Did the originally panel (Version 1) chosen by government scientists actually include Mycobacterium tuberculosis and related microbes in its design — only to find that indeed these mycobacteria caused positive tests for Ebola as in the HIV affair? Did they feel that such results might muddy the waters, be too difficult to explain, and subsequently remove them? This is not known.
Therefore are the HIV drugs working
against an “Ebola” which is estimated to have killed well over
3,000 African’s so far this year or the TB that killed 600,000
Africans in that same window? There still remains much work ahead to
determine this. Antiretrovirals have major side effects. “Angola is in the grip of the world’s worst ever outbreak of the Marburg virus. According to the World Health Organization (WHO), as of 5 April, 156 of the 181 people reported infected have died. The Ebola-like virus causes a fever that, in fatal cases, is usually accompanied by severe internal bleeding and shock. There is no vaccine or medical treatment and up to 80 per cent of infected people die within three to seven days. Three-quarters of those affected are children under five. Diagnosing an infection with the Marburg virus can be difficult as its initial symptoms are similar to those of malaria or tuberculosis. They include diarrhea, stomach pains, nausea, and vomiting and severe chest pains.”35 The heavy mortality and morbidity under the age of five with Marburg brings to mind specifically a tubercular involvement, in which most children are affected also in the same age group. What has been called ‘The Golden Age of Resistance’ against TB mortality has always been, for unknown reasons, ages six thru fifteen.4 In this same vein, during the Zaire Ebola outbreak of 1976, women 15-29 years of age had the highest incidence of that disease.36 “We saw a gigantic worm like-structure — gigantic by viral standards. It’s a very unusual shape for a virus” Peter Piot.
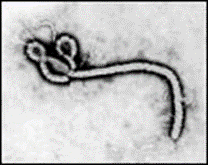
Figure
4. The Serpentine Form of the Ebola Virus. Magnification:
approximately x60,000.
To some it might be considered “worm-like”, to others serpentine.
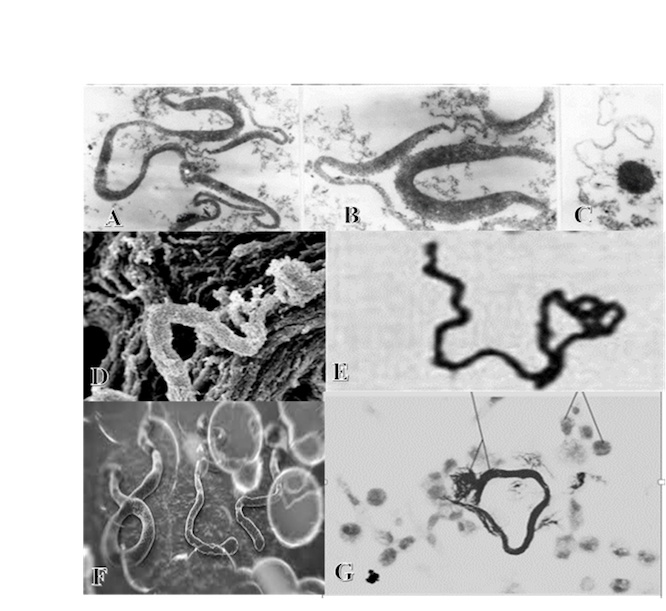
TB OR EBOLA?
Figures 5A through 5G. Which of the serpentine, worm-like forms above is the Ebola virus?The correct answer is Figure 5 F. Figures 5A,5B and 5C are L-Forms (Or Cell-Wall-Deficient Forms) of TB Under theElectron Microscope. (Michailova, L et al. Morphological variability and cell wall deficiency in ‘heteroresistant’ strains. Internat Journ of Tuberc and Lung Dis, 9:,8, Aug 2005:.907-914:,911). Figure 5D. Worm-like lethal tubercular cords from an atypical TB under the Electron Microscope. (Julián E, Roldán, M Journ. Of Bact Apr. 2010 p.1751-1760. P.1756). Such virulent cords are also represented in Figure 5E (Darzins, E. The Bacteriology of Tuberculosis Minneapolis. 1958. 488pps. p296) and Figure 5G.
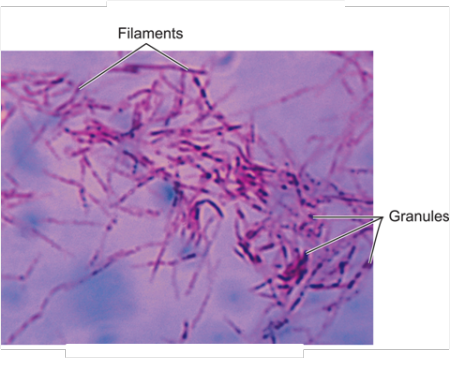
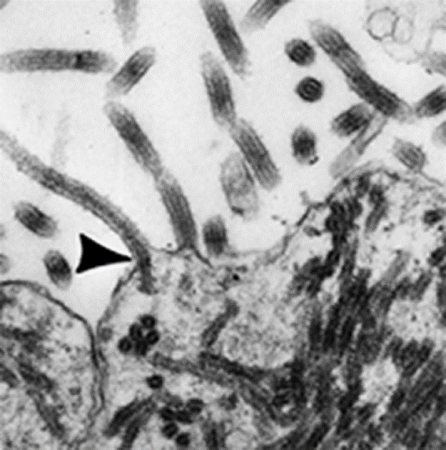
Both the Ebola virus and the Marburg virus are called Filoviruses because they form filamentous infectious viral particles. Filoviruses, however, are not alone. Mycobacterium. tuberculosis, which commonly lodges in and multiplies in the white cell defenders of our body (called macrophages) — also become filamentous once inside a macrophage.37 (See figures 6,7)
Figure .6 Filamentous Cell-Wall-Deficient Forms of Mycobacterium tuberculosis
Figure 7.
Filamentous Forms of the Ebola. Magnification: approximately x40,000.
WHO’s statement is misleading. As far back as 1995 the ability of Ebola to aerosolize or spread through airborne transmission was reported, studied and confirmed.39,40 Ebola, is a communicable airborne infection, just like tuberculosis.
Tubercular Monkeys, Apes and Fruit Bats
It is felt that the new strain probably arrived in West Africa via infected straw-colored fruit bats from another part of Africa and seems to be related to that Zaire Ebola virus identified more than 10 years ago in the Congo. These bats migrate across long distances and are commonly found in giant colonies near cities and in forests. Fruit bats, however, are widely eaten in rural West Africa supposedly as a delicacy. But the same fruit bats can carry mycobacteria from the mycobacterial tuberculosis complex.44,45,46 Previous Ebola outbreaks saw catastrophic death rates in gorilla and chimpanzee populations, which led some scientists to think that they were the ones responsible for the disease spreading. Old World monkeys are very susceptible to human and cattle tuberculosis. Unlike humans, monkeys have no natural resistance to the disease. When they do catch it from a human, it usually spreads very fast and fatally in their bodies (as in acute miliary tuberculosis) and to areas other than their lungs. During their illness, they can spread the disease to anyone who comes in contact with them or their waste.
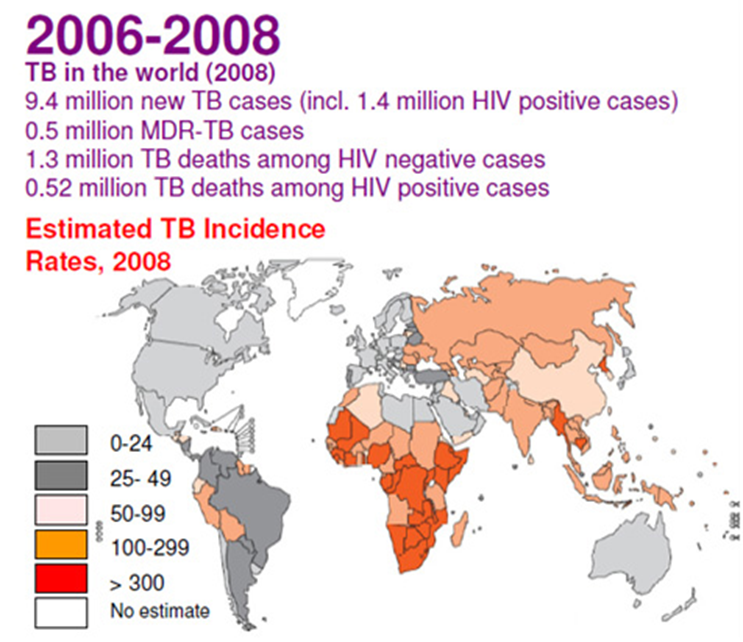
The current Ebola virus began in West Africa, a hotbed of tuberculosis. (See Figure 8)
Figure 8: Map showing the true severity of the tuberculosis problem; in 2006-2008 - the last period before WHO's TB statistics dived as a result of including many TB cases into the wastebasket of "AIDS-defining illness". Note that the darker-colored regions are mostly in Africa. (Source: WHO
Another map recently put out by WHO lumps Ebola deaths in West Africa under the puzzling single category “probable, confirmed, and suspected”.47
REFERENCES:
Dr. Lawrence Broxmeyer, MD See Also: Broxmeyer, L. AIDS: What the Discoverers of HIV Have Never Admitted: Latest Edition. 2014, July. 142 pp.
Pennsylvania internist/researcher Lawrence Broxmeyer, MD, was on staff at N.Y. affiliates of Downstate, Cornell, and NYU for 14 years. He was lead author and originator of a novel way to kill AIDS mycobacteria. (Journal of Infectious Diseases, 11/15/2002}. His ideas on phagotherapy are still in use today. He appeared in Patho-Biotechnology, by Landes. His peer-reviewed articles are on PubMed. His books include "Parkinson’s—Another Look", "Autism: An ancient Foe" and "AIDS: What the Discoverers of HIV Have Never Admitted." SEE: AIDS: What the Discoverers of HIV Have Never Admitted: Latest Edition
|
| Donate
to Rense.com
Support Free And Honest
Journalism At Rense.com |
Subscribe
To RenseRadio!
Enormous Online Archives,
MP3s, Streaming Audio Files,
Highest Quality Live Programs |
 The CDC (Centers for Disease Control and Prevention) recently declared:
The CDC (Centers for Disease Control and Prevention) recently declared: